introduction
Imagine being diagnosed with a disease that you may live with for decades—or one that could suddenly become aggressive overnight. That’s the unpredictable reality of Chronic Lymphocytic Leukemia (CLL), the most common type of leukemia in adults. In 2025, groundbreaking research is rewriting the playbook on how we understand, diagnose, and treat this enigmatic blood cancer. From genetic discoveries that predict disease aggression to therapies that reprogram the immune system, this article uncovers the latest breakthroughs every patient needs to know. Buckle up: what you’re about to read could change how you view CLL forever.

Don’t shy to share
1. What Is CLL? Understanding This Mysterious Blood Cancer
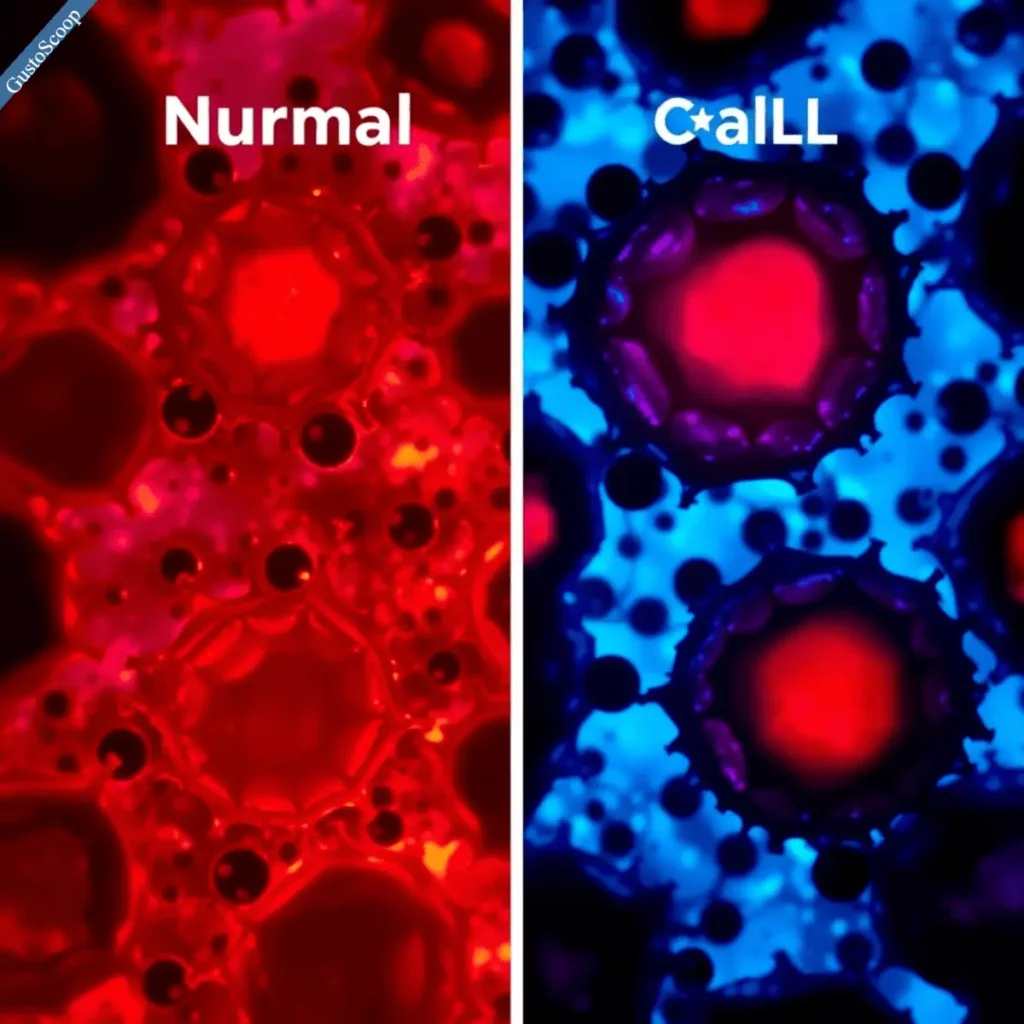
CLL is a slow-growing cancer that targets B lymphocytes, white blood cells essential for fighting infections. Unlike aggressive leukemias, CLL often lurks silently, with some patients going years without symptoms. But don’t be fooled—its unpredictability is its hallmark.
How is CLL different? While acute leukemias like AML explode rapidly, CLL creeps. However, it can morph into Richter’s transformation, a fast-moving lymphoma, in 5-10% of cases.
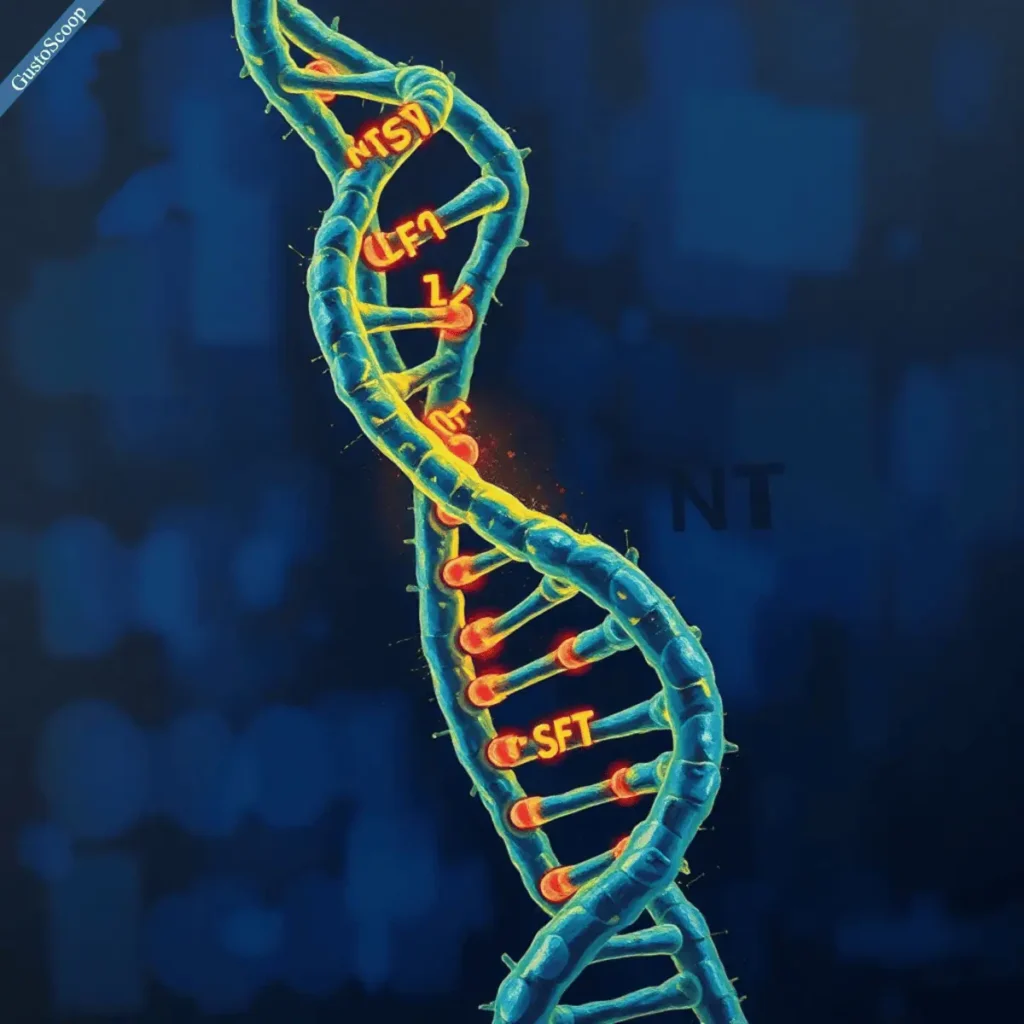
New Genetic Clues: A 2024 New England Journal of Medicine study revealed that mutations in TP53 or NOTCH1 genes act as “crystal balls,” predicting aggressive progression. Researchers also found that deletions in chromosome 17 correlate with treatment resistance. “These markers help us stratify patients early,” says Dr. Susan O’Brien, a leading CLL oncologist.
2. How Fast Does CLL Progress? The Truth About Disease Stages
CLL’s speed varies wildly. Doctors use Rai (0-IV) and Binet (A-C) staging systems to gauge risk. Early-stage patients (Rai 0) might never need treatment, while advanced stages (Rai III/IV) demand immediate action.
The Richter’s Wild Card: About 5% of patients face Richter’s transformation, where CLL becomes a deadly lymphoma. A 2023 Blood journal study tied this shift to SF3B1 and BRAF mutations.
Shocking Speed: A 2025 Mayo Clinic trial found that patients with double-hit mutations (e.g., TP53 + NOTCH1) progress 3x faster than others. Genetic testing is now a non-negotiable step in diagnosis.
3. The Scariest Leukemia: How Does CLL Compare to Other Types?
AML is often dubbed the “deadliest” leukemia, with a 5-year survival rate of 29% vs. CLL’s 87%. But CLL’s Jekyll-and-Hyde nature terrifies patients. It can idle for years, then turn lethal without warning.
Survival Stats Update:
CLL: 87% 5-year survival (SEER 2023 data).
AML: 29% (same dataset).
Richter’s transformation: Drops survival to under 1 year in 50% of cases.
“CLL’s unpredictability keeps us humble,” admits Dr. John Byrd of Ohio State University.
4. Can You Cure CLL? The Hope (and Limitations) of Modern Medicine
No cure exists yet, but treatments now control CLL like never before. BTK inhibitors (e.g., ibrutinib) and BCL-2 blockers (venetoclax) have revolutionized care.
CAR-T Cell Therapy Breakthrough: A 2025 phase III trial in Lancet Oncology showed CAR-T therapy achieved complete remission in 52% of high-risk CLL patients. “We’re seeing responses we never thought possible,” says trial lead Dr. David Porter.
5. How Long Can You Live with CLL? New Data on Survival Rates
Survival hinges on genetics and stage:
Low-risk CLL (no TP53/mutated IGHV): Median survival 15+ years.
High-risk (TP53/del17p): Median survival 2-4 years without novel therapies.
Future Projections: Dr. Nicole Lamanna of Columbia University predicts, “By 2030, targeted therapies could push 10-year survival past 90%.”
6. Early Warning Signs of CLL: Symptoms That Shouldn’t Be Ignored
Early symptoms are subtle: fatigue, painless swollen nodes, or frequent colds. But red flags like drenching night sweats, unexplained 10% weight loss, or a swollen spleen demand urgent care.
Case Study: Sarah, 47, ignored fatigue and recurrent sinus infections for a year. By diagnosis, her CLL had advanced to Binet Stage C. “I wish I’d pushed for blood tests sooner,” she says.

7. How to Naturally Reduce Lymphocyte Counts in CLL
While diet won’t cure CLL, studies suggest:
Anti-inflammatory foods: Turmeric, fatty fish, and berries lower cytokines linked to CLL growth (Cancer Research 2023).
Fasting Mimicking Diets: A 2024 Nature study found 5-day fasting cycles reduced lymphocyte counts by 30% in mice with CLL.
“Lifestyle tweaks complement meds but aren’t substitutes,” warns nutritionist Dr. Nasha Winters.
Don’t shy to share
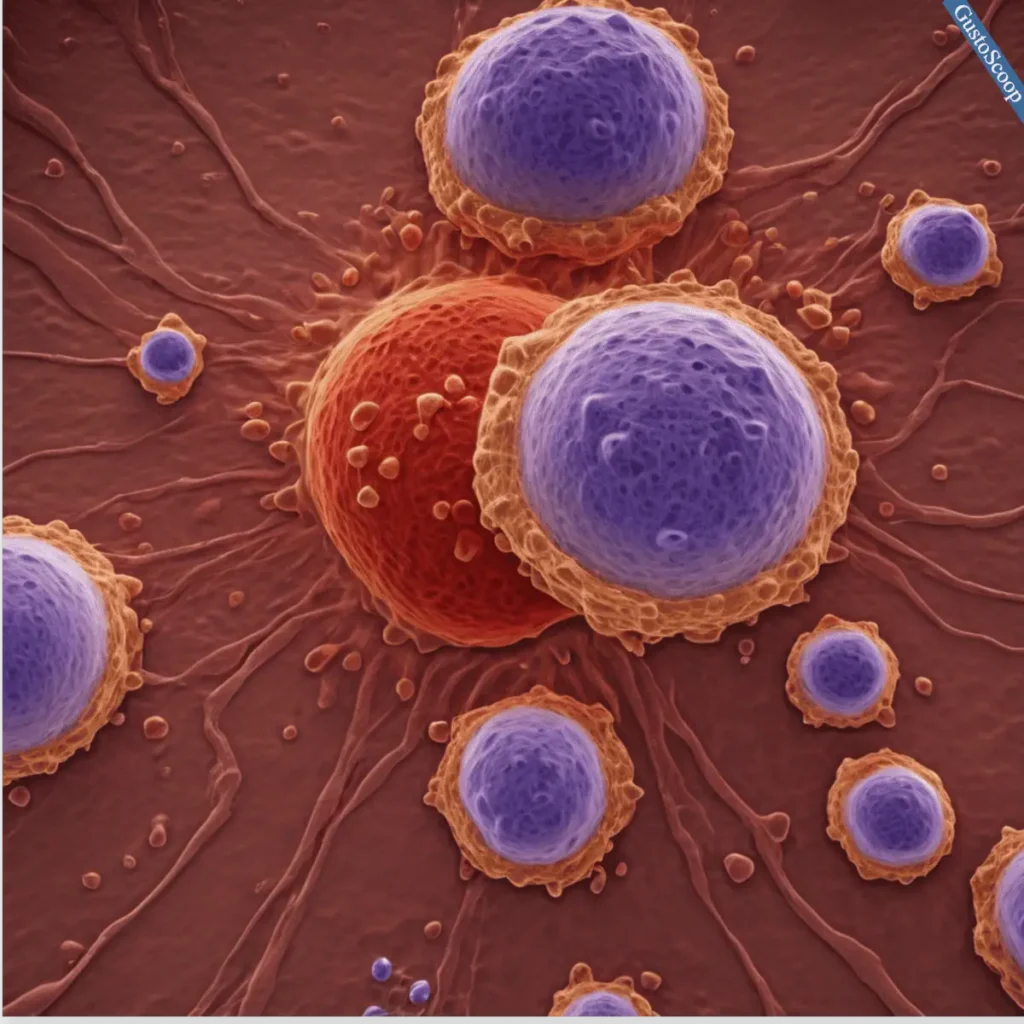
8. What Happens to B Cells in CLL? The Science Behind the Disease
CLL hijacks B cells, turning them into lazy, infection-fighting failures. These malignant cells overcrowd bone marrow, causing anemia and immune collapse.
New Drug Alert: Pirtobrutinib, a next-gen BTK inhibitor, targets resistant CLL cells. A 2025 JAMA Oncology trial reported 68% response rates in patients who failed prior therapies.
9. End-of-Life Signs in CLL: How to Recognize When the Disease Is Advancing
Final-stage signs include relentless fatigue, recurrent sepsis, and plummeting blood counts. Palliative care teams can ease symptoms with transfusions, pain management, and emotional support.
Pro Tip: Early hospice referral improves quality of life, per a 2024 Journal of Clinical Oncology study.

10. The Future of CLL Research: What’s Coming Next?
AI Diagnostics: MIT’s 2025 algorithm predicts Richter’s transformation 6 months earlier than current methods.
Drugs to Watch: Non-covalent BTK inhibitors and CD19-targeted bispecific antibodies are nearing FDA approval.
Don’t shy to share
Conclusion
CLL remains a complex foe, but 2025’s research offers unprecedented hope. From genetic testing to CAR-T breakthroughs, patients have more tools than ever. Stay informed, advocate for cutting-edge care, and ask your doctor about clinical trials. As Dr. William Wierda of MD Anderson urges, “Today’s trials are tomorrow’s cures.”
Your Next Step: Download the latest CLL guidelines from the Leukemia & Lymphoma Society and discuss them at your next appointment. The future of CLL care is brighter—and it’s yours to seize.
FAQ :
In most countries, the very first shot is the Hepatitis B vaccine, usually given within the first day after birth. Doctors start Hepatitis B in the hospital because a baby can catch this virus from the mother during delivery. This early dose begins protecting the infant’s liver right away.
Yes – it’s common for babies to get multiple shots in one visit and it is safe. New vaccines are tested together with existing ones to make sure they don’t interfere. In fact, co‑administering shots helps protect babies sooner and spare extra visits.
The timing between doses is based on how the immune system responds. Vaccine schedules are designed so each shot has time to work. For example, CDC notes that if two live vaccines (like MMR and chickenpox) aren’t given on the same day, you should wait at least 4 weeks between them. In general, clinical trials set these intervals so that each dose produces a strong immune response and long-lasting protection.
In the U.S., the CDC schedule starts at birth and continues through the first year. A newborn gets Hepatitis B in the hospital, then follow-up doses of various vaccines at 2, 4, and 6 months (for DTaP, Hib, polio, pneumococcus, rotavirus, etc.), and then boosters like MMR (measles/mumps/rubella) and chickenpox around 12–15 months. This timetable matches the ages when babies are most vulnerable to specific diseases.
Babies need protection against many different diseases, and each vaccine usually requires a series of doses. For example, at the 2-month visit a baby typically receives shots for DTaP (diphtheria, tetanus, whooping cough), Hib, polio, hepatitis B, pneumococcus, and rotavirus. Giving multiple vaccines together is how immunizations “work best to safely and effectively build your child’s immunity against many serious illnesses”.
Yes. According to the CDC, “vaccines are very safe” and the U.S. has the safest vaccine supply ever. Millions of babies get immunized each year with only very mild reactions (like a low fever or sore arm) in most cases. Serious reactions are extremely rare.
Doctors advise not to delay. Sticking to the recommended schedule keeps babies protected when they’re most at risk. Spreading out or postponing vaccines only leaves a baby vulnerable to diseases for longer – there’s no safety benefit to delaying. In other words, any time off the schedule is time without protection.
Early childhood vaccines guard against many serious infections. For example, the routine shots protect against whooping cough (pertussis), diphtheria, tetanus, polio, Haemophilus influenzae type b (Hib), pneumococcal infections, rotavirus, and hepatitis B. By the time kids are a year old they’re also protected from measles, mumps, rubella and chickenpox (varicella)cdc.gov. Staying up to date on these vaccines keeps dangerous childhood diseases rare.

